As the new year approaches and New Year’s resolutions find their way into journals and calendars, healthcare providers need to consider how we may best support our patients on their journeys in 2022. A popular resolution that will surely find its way to the patients in our care will be around weight.
The conversation around weight starts an inevitable cascade of data points, risk factors, and statistics within the minds of healthcare providers. We’ve repeatedly heard the connection between chronic disease and weight, yet we haven’t cracked the code and found a universal way to support patients.
What if we, as contributing members of the healthcare system, decide to approach weight differently? What if we decide what we’ve been doing isn’t working and seek a different way to support our patients? What if our own New Year’s resolution is to shift our own perception, so our patients receive the best possible care?
A fresh perspective
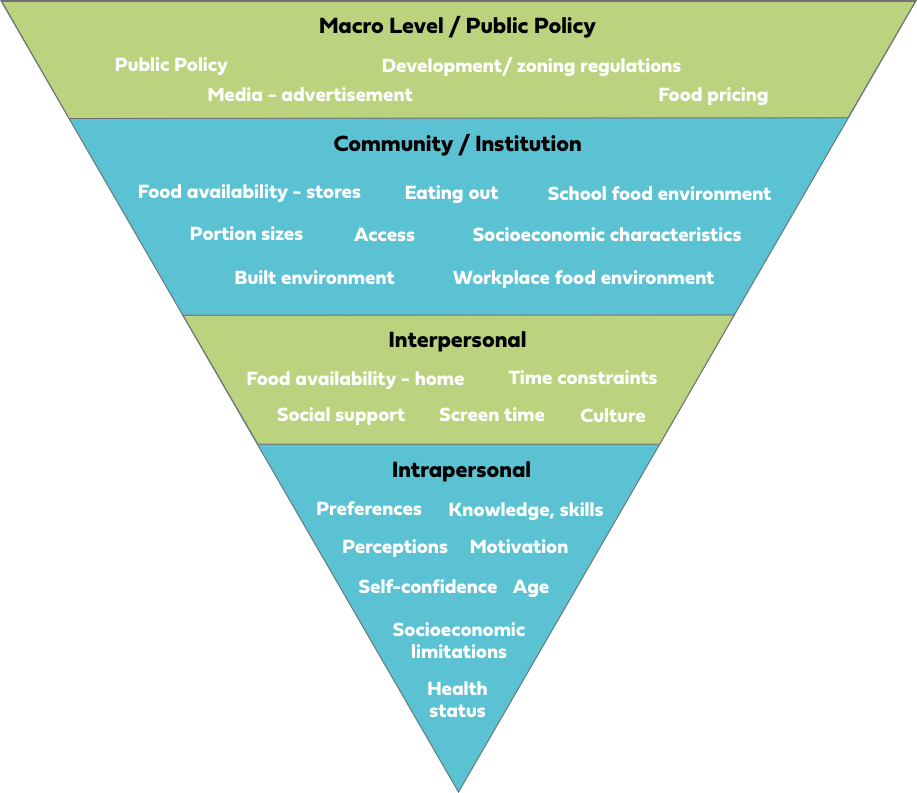
One powerful place to start is to acknowledge the complexity of weight and that personal and individualized care should find its way into the weight conversation. Weight is complex.Everything from the family unit to the design of the city in which our patients live has an impact. It is a result of behavior, genetics, society, education, marketing, and so much more!
Improving the patient experience
It’s important to remember that the number on the scale is the least interesting thing about a person.
And yet, in a healthcare setting, the scale is often the first experience our patients have in our care. While operationally this may make sense for the flow of the care center, patients might feel as if the appointment will be dictated based on that number. While we may be unable to change the flow of the appointment (or can we?!), we can shift the patient experience. If taking a patient’s weight is part of the appointment, consider incorporating the following:
- Ask the patient about the best part of their day, their weekend plans, or something they’re looking forward to. “What are you most looking forward to this week?”
- Recognize the patient for something not related to numbers. “That scarf is so bright and cheery!”
- If a patient comments on their weight, normalize the fact that weight fluctuates. “I hear what you’re saying and would like to share that the number on the scale is one part of your health, not the end-all-be-all determinant of it. Weight is meant to fluctuate.”
 Examining our perceptions
Examining our perceptions
An important way to increase our success with these conversations is to recognize our own perception of weight.
Ask yourself: How might my own beliefs influence the care I provide?
Consider following this link and exploring the Weight Implicit Association Test (IAT) from Project Implicit. Project Implicit is a non-profit organization founded in 1998 to research and educate people around biases. Understanding our own ideas on the topic of weight can allow us to provide an improved experience for our patients.
 Discussing behavioral changes
Discussing behavioral changes
So how can we meet patients where they are and support them?
While our patients may set goals around the number on the scale, as medical providers, we need to remember weight is an outcome and does not deserve to be the focus. We need to shift the language we use when discussing behavior change with patients. What if, instead of talking to patients about “losing weight,” “increasing exercise,” or “eating healthier,” we explore the behaviors and strategies that might support those outcomes?
 “What kinds of movement or exercise do you enjoy? What have you enjoyed in the past? What do you like about it? What helps you to incorporate this into your day/week?”
“What kinds of movement or exercise do you enjoy? What have you enjoyed in the past? What do you like about it? What helps you to incorporate this into your day/week?”- “What kinds of foods do you like to eat? What makes your meal or snack time enjoyable for you? What new recipe or food might you try?”
- “You shared that you want to lose weight. What would that change make possible for you?”
- “What have you done in the past that may be helpful in the future?”
In a traditional appointment, you may find you’re unable to explore all of these questions, but what if you simply explored one question? How might that shift the trajectory of the appointment and the care your patient receives?
Supportive team members can make a difference
If you’re lucky enough to have a certified health coach or registered dietitian as part of your team, utilize their expertise! They can support your patients in achieving their desired outcomes by spending time exploring behaviors. All Vera patients and care centers have access to health coaching services, and these behavior change experts are just waiting to support you — let them!
As 2021 comes to a close, and we look ahead to 2022, let us consider how we might support our patients differently in conversations around weight. Perhaps this is the year we make a bold shift, a change in our approach, and see if we get a different outcome. What new strategy or behavior might you put into action?
Resources
Fitzgerald, Nurgul & Spaccarotella, Kim. (2009). Barriers to a Healthy Lifestyle : From Individuals to Public Policy — An Ecological Perspective. Journal of Extension. 47. 1FEA3.
Moore, M., Jackson, E., & Tschannen-Moran, B. (2016). Client Assessment. In Coaching psychology manual. essay, Wolters Kluwer.
Nutrition and Weight Status. (n.d.).
Sign up
Join our email list to receive the latest open positions, Vera Careers news, and more.






