This is the perfect time to plan your benefit strategy for the second half of 2022 and beyond. Competitive benefits programs are more important than ever, as the pandemic and Great Resignation continue to cause unprecedented changes to workforces and the economy.
Yet, rising healthcare costs make effective benefit planning a challenge that can, at times, feel impossible. Across the country, industry leaders are searching for new, cost-effective solutions to assist them in recruiting and retaining talent. There’s also more emphasis than ever on the importance of member utilization, as well as mental and emotional well-being.
What does an effective benefits plan look like?
Modern benefit strategies need to be meaningful, so plans can improve overall health, drive down total cost of care, and keep employees satisfied.
Driving down total cost of care might seem like a tall order, as healthcare costs continue to reliably balloon upward each year. Larger organizations, on average, have seen the price of their plans increase by 15% each year. If nothing changes, they can expect that trend to continue.
Unfortunately, those rising costs don’t always lead to improved outcomes in member physical, mental, and emotional health. They’re also not guaranteed to keep them engaged and satisfied. Deeper investigation is required to discern which benefit options add the greatest value, as opposed to merely maintaining the status quo.
When determining how a benefits plan can meet the needs of your population, take stock and ask yourself:
- What does our population do?
- What do their lives look like?
- What will be meaningful to them and how can a benefits solution align with that?
- Are there places where we can eliminate redundancies and add value?
Connecting the pieces
 While there’s no shortage of options available these days, many groups end up with fragmented approaches. While a number of rich benefit options might exist, they aren’t coordinated enough or well connected. Utilization can also be low, due to confusion amongst members, a lack of meaningful relationships with their care team, or a lack of incentives.
While there’s no shortage of options available these days, many groups end up with fragmented approaches. While a number of rich benefit options might exist, they aren’t coordinated enough or well connected. Utilization can also be low, due to confusion amongst members, a lack of meaningful relationships with their care team, or a lack of incentives.
Comprehensive design is of vital importance in solving these issues. While there are reasons and arguments for providing options within tiered plans, or including additional options to drive utilization, a successful plan must include a centralized form of care navigation.
When it’s time to redesign
If you’ve continued to watch costs rise, while feeling helpless to address them, then it’s time to consider revisiting the design of your benefits plan. Options are available to stop the rate of inflation and allow you to access fixed and predictable primary care costs.
Perhaps you’ve also wondered whether any alternatives are available that would allow you to improve employee health. The greatest asset of any organization is its people, and many businesses are realizing that benefits are about more than attracting and retaining talented employees. They’re also about creating something better for your people.
Plans that keep employees satisfied
There are many factors affecting employees’ satisfaction with their benefits, including flexibility and access to care. Like their employers, employees are especially concerned about rising costs of healthcare, while hoping their benefits will provide a meaningful level of care.
Meaningful care is about more than addressing occasional health concerns or getting access to help during emergencies. Most people find meaning in continuity, when they’re able to build trusted relationships with their providers. Unfortunately, a number of people don’t have access to a medical home. This means they end up with gaps in their care and less access to preventative solutions.
Proactive care vs. reactive care
 In recent years, COVID-19 has revealed the critical importance of ensuring that people have access to primary care resources and a medical home. Primary care can even solve for the unexpected, helping in ways beyond what most people realize. Throughout the pandemic, Vera Whole Health has partnered with employers and human resource departments:
In recent years, COVID-19 has revealed the critical importance of ensuring that people have access to primary care resources and a medical home. Primary care can even solve for the unexpected, helping in ways beyond what most people realize. Throughout the pandemic, Vera Whole Health has partnered with employers and human resource departments:
- Keeping them up to date with pandemic guidelines
- Helping with return-to-work protocols
- Assisting with vaccinations
- Consistently providing members access to high-quality primary care
The power of creative solutions
 To create impactful benefits plans, employers must clarify their end goals, search for new solutions, and determine which of those solutions will meet their needs. Right now, there’s a lot of opportunity for groups to bring creative solutions to the table rather than remain with what’s comfortable.
To create impactful benefits plans, employers must clarify their end goals, search for new solutions, and determine which of those solutions will meet their needs. Right now, there’s a lot of opportunity for groups to bring creative solutions to the table rather than remain with what’s comfortable.
Incentives are emerging as a popular strategy for improving engagement. Innovatively incentivising around benefit designs, after investing in a primary care solution, can be a big source of encouragement for members. It’s also a great way for leadership to demonstrate their commitment to, and belief in, the solutions they’re offering.
There are often two common perspectives when it comes to benefit design, a transactional lens and a cultural lens.
- The transactional lens can lead to decisions that might seem better in the short term but don’t creatively address long-term problems.
- The cultural lens leads to creative solutions, better outcomes, and reduced total cost of care. Rather than focusing only on immediate concerns, it considers the benefits of consistency, increased engagement, and improved satisfaction.
How advanced primary care (APC) brings it all together
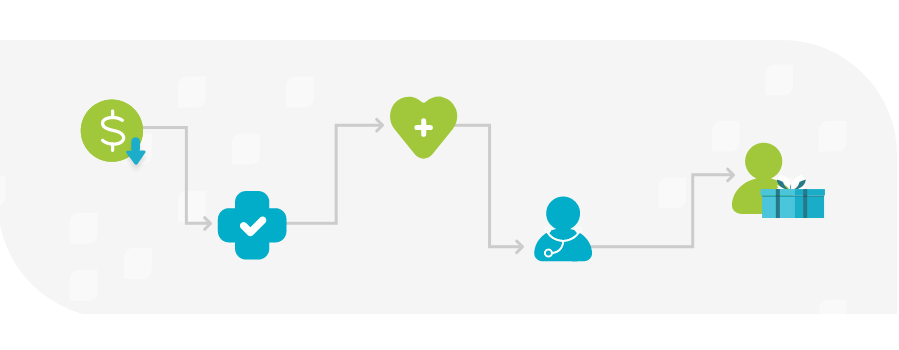
 Vera’s APC model addresses the downfalls of a fragmented approach to healthcare by giving members access to a trusted medical home. When APC isn’t at the center of value-based plans, it means no one is at the helm guiding the ship through uncertain waters. But, when APC serves as a primary touchpoint and navigator through each employee’s healthcare journey, people understand their options better, can make educated decisions, and become better consumers of their own healthcare plans.
Vera’s APC model addresses the downfalls of a fragmented approach to healthcare by giving members access to a trusted medical home. When APC isn’t at the center of value-based plans, it means no one is at the helm guiding the ship through uncertain waters. But, when APC serves as a primary touchpoint and navigator through each employee’s healthcare journey, people understand their options better, can make educated decisions, and become better consumers of their own healthcare plans.
APC is also the solution to wasteful spending. It addresses rising costs and allows for better insight into finances for future budgeting. When primary care is high-quality and easy to access, expensive and harmful health crises are also reduced.
Vera care teams improve clinical outcomes in a number of ways, including the use of comprehensive, annual health evaluations. These evaluations allow them to build strong relationships with their patients, look at historical claims information, ask the right questions, and close care gaps and referral loops. Unlike many traditional fee-for-service models, providers also follow up with members and actively coordinate their care.
But, that’s only the beginning of what Vera provides. Access to Vera Whole Health coaches, an emphasis on empathetic listening, and longer appointment times all contribute to improved health outcomes.
Reflecting your values
When redesigning your benefits program, ask yourself what your organization’s mission and values are. Do your benefits match up to those? Do they demonstrate to your employees that their health is a priority? With Vera’s APC model, you have a comprehensive tool at your disposal to address rising costs, while doing exactly that.
